
Made possible with support from Blue Shield of California Foundation and the California Health Care Foundation.
BRIEF | JULY 2019
Exploring the Impact of Integrated Medicaid Managed
Care on Practice-Level Integration of Physical and
Behavioral Health
By Logan Kelly, Michelle Conway,
*
and Michelle Herman Soper, Center for Health Care Strategies
IN BRIEF
Clinical integration of physical and behavioral health services may improve health outcomes and reduce costs for
individuals with behavioral health conditions, but separate Medicaid financing for physical and behavioral health
care can create barriers to coordinated care delivery. In recent years, several states have begun contracting with
comprehensive managed care plans to integrate behavioral health services and reduce the fragmentation of care
for Medicaid enrollees. This brief, produced with support from Blue Shield of California Foundation and the
California Health Care Foundation, describes how integrated financing influences the coordination of physical and
behavioral health services at the care delivery or practice level. It distills insights from providers in three states —
Arizona, New York, and Washington — that have recently transitioned to integrated managed care. Based on their
insights, the brief highlights recommendations for states seeking to improve health outcomes through advancing
greater physical-behavioral health integration organized within three key areas: (1) data and quality measures; (2)
payment and business practices; and (3) integrated clinical service delivery.
Background
Health Impacts and Costs of Behavioral Health Conditions
People with behavioral health conditions — those with mental health and/or substance use
disorders (SUD) — are more likely to experience poor health and social outcomes as well as high
costs of care.
1
They have higher rates of chronic physical conditions, as well as increased rates of
homelessness, unemployment, poor educational performance, and involvement with the criminal
justice system.
2
Strikingly, people with serious mental illness (SMI) die on average 25 years earlier
than those without SMI.
3
Medicaid is the single largest payer for behavioral health services in the United States, with nearly 20
percent of Medicaid enrollees having a behavioral health diagnosis.
4
Medicaid spending for
enrollees with behavioral health conditions is more than four times higher than those without these
conditions, largely as the result of increased physical health care spending.
5
One study found that
over 80 percent of the increased costs for people with comorbid mental and physical health
conditions were associated with physical health expenditures.
6
*
Michelle Conway is a former intern at the Center for Health Care Strategies.
BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 2
Despite the connections between behavioral and physical health conditions, many Medicaid
enrollees experience gaps in care due to the lack of coordination and information sharing between
medical and behavioral health providers, which can result in adverse outcomes for patients with
comorbid conditions. People with behavioral health conditions also tend to receive less preventive
care and lower-quality physical health care, a disparity that may be affected by the stigma associated
with behavioral health conditions.
7
Physical-Behavioral Health Integration
Many physical and behavioral health providers say that integrated care better meets the needs of
patients with multiple co-occurring conditions. Integrated behavioral health care (integrated care) is
defined by the Agency for Healthcare Research and Quality as: “the care a patient experiences as a
result of a team of primary care and behavioral health clinicians, working together with patients and
families, using a systematic and cost-effective approach to provide patient-centered care for a
defined population. This care may address mental health and substance abuse conditions, health
behaviors (including their contribution to chronic medical illnesses), life stressors and crises, stress-
related physical symptoms, and ineffective patterns of health care utilization.”
8
Clinical integration references processes to advance integrated care at the point of service delivery,
and is often represented as a continuum beginning with coordinated care and then co-located care,
with the highest level defined as full collaboration in a transformed/merged integrated practice.
9
While clinical integration can be implemented in different settings that serve different populations,
integration of behavioral health into primary care settings most frequently targets people with mild
to moderate mental health conditions. Integration of primary care into behavioral health settings
targets adults with SMI and SUD and children with serious emotional disturbances (SED) who may
have high levels of physical health comorbidities. There is growing evidence that clinical integration
can improve health outcomes and quality of life as well as reduce health care costs.
10
Many states
have initiated efforts to pursue clinical integration, especially for vulnerable populations of high-need
Medicaid enrollees.
11
One barrier states face in advancing clinical integration for Medicaid enrollees is separate financing
structures for physical and behavioral health care. For many years, most states with Medicaid
managed care programs have “carved-out” behavioral health benefits from physical health benefits.
While the majority of states organize and finance physical health benefits through comprehensive
managed care organizations (MCOs), mental health and SUD services have been administered by
separate managed behavioral health organizations (which are often public entities) or on a fee-for-
service basis. Under such systems with a person’s care managed by multiple entities, consumer
access to care and care coordination can be diminished, resulting in worse health outcomes.
12
In recent years, several states have transitioned to integrated financing models by contracting with
integrated managed care plans that manage all physical and behavioral health services for Medicaid
enrollees, to decrease fragmentation of care, improve health outcomes, and reduce costs. A primary
goal of these programs is to enhance providers’ access to data, incentives, and tools to deliver
integrated services and coordinate care across settings. The potential of integrated physical-
behavioral health financing to improve care and outcomes hinges on whether the integration of
BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 3
financing supports integration at the clinical level, and whether consumers — particularly those with
complex health and social needs — receive care that is better coordinated.
To examine whether integrated financing is delivering on the promise of improved clinical
integration and coordination at the practice level, the Center for Health Care Strategies (CHCS), with
support from Blue Shield of California Foundation and the California Health Care Foundation,
conducted interviews with leaders of nine provider organizations in three states — Arizona, New
York, and Washington — that have implemented integrated Medicaid managed care programs.
Most interviewees reported that their state’s movement toward plan-level financial integration has
accelerated their organization’s clinical integration progress. Providers identified three key levers for
successfully advancing integrated care that are described in this brief:
1. Integrated data-sharing and quality measures to use with plans and providers;
2. Payment and business practices that align financial incentives for providers to deliver
integrated care, including adoption of value-based payment arrangements; and
3. Integration in clinical service delivery, including adoption of clinical practices that foster
integrated care delivery, such as service redesign, assessments, staffing, and care planning.
Whereas the overall feedback from interviewees highlights the promise of financial integration,
many providers also identified challenges and unintended consequences resulting from the design
and implementation of state transitions to integrated financing. This brief shares insights from both
positive and negative experiences that can inform future state efforts to advance clinical integration.
Recommendations for other states seeking to advance integration follow each of the three thematic
sections. These recommendations identify critical decisions for states related to both the design of
integration policies and the transitions to and ongoing monitoring of integrated managed care
programs.
Profiled States and Providers
This brief draws on interviews with providers in Arizona, New York, and Washington. These states
were selected based on their recent and diverse approaches, as summarized below, to implementing
integrated managed care. (See Appendix 1 for additional details about each state’s transition,
including a timeline and description of how providers were paid during each phase.)
Arizona
In 2013, Arizona’s state Medicaid agency, the Arizona Health Care Cost Containment System
(AHCCCS), began integrating the financing of physical and behavioral health services for certain
populations. Before 2013, MCOs were primarily responsible for physical health services, while most
Medicaid behavioral health services were carved out of AHCCCS Medicaid MCO contracts, and
separately managed by Regional Behavioral Health Authorities (RBHAs). Through a geographically
phased rollout that launched in 2014, newly integrated RBHAs began managing physical and
behavioral health services for adult Medicaid enrollees with SMI. In 2018, integrated AHCCCS
Complete Care (ACC) plans began managing both physical and behavioral health services for enrollee
populations that previously enrolled in separate plans, including: (1) children with SED; (2) adults
BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 4
with SUD; and (3) adults and children with mild-to-moderate behavioral health needs. An evaluation
of 2013-2014 integration initiatives found improvement in all measures of patient experience,
ambulatory care, preventive care, and chronic disease management. Hospital-related measure
results were mixed, however. While the majority of these measures, such as 30-day post-
hospitalization for mental illness follow up rate, showed improvement, some measures such as
inpatient utilization rate showed a performance decline.
13
New York
Prior to 2015, most specialty behavioral health services in New York were carved out of managed
care plans and provided via fee-for-service. In 2015, New York began transitioning all adults eligible
for Medicaid managed care to receive physical and behavioral health benefits from an integrated
managed care plan, and created a new type of health plan, called a Health and Recovery Plan
(HARP). HARPs are separate products within existing MCOs for adults with SMI and serious SUD
diagnoses, and have additional requirements for care management and newly added home- and
community-based services benefits. New York is phasing in integrated managed care plans and
HARPs for children in 2019, along with expanding covered mental health and SUD services for
children and their families. New York issued a request for proposals in January 2019 to evaluate this
behavioral health demonstration, including improvements in health and behavioral health outcomes
for enrollees in integrated MCOs.
14
Washington
Before 2016, three separate entities managed physical and behavioral health care in Washington:
(1) all physical health as well as behavioral health services for individuals with mild to moderate
needs were managed by MCOs; (2) specialty mental health services for enrollees with SMI were
managed by Regional Support Networks (RSNs) that subcontracted with community mental health
agencies to deliver care; and (3) SUD services were administered through multiple regional and state
contracting mechanisms. In 2016, the Washington Health Care Authority (HCA) began implementing
fully integrated managed care, phased in by region. Under the fully integrated managed care model,
MCOs provide physical and behavioral health services to adults and children, while the state
contracts with administrative service organizations in every region to deliver crisis services to
Medicaid and non-Medicaid enrollees. An evaluation of integration efforts for adult populations in
an early adopting region found statistically significant improvement in 10 out of 19 enrollee
outcomes in 2016 and 11 out of 19 enrollee outcomes in 2017, including access to preventive/
ambulatory health services, SUD treatment penetration, and mental health treatment penetration.
15
Most other outcomes did not show significant relative change, though two outcomes
(comprehensive diabetes care — hemoglobin A1C testing and emergency department (ED)
utilization per 1,000 coverage months) showed statistically significant unfavorable changes. Notably,
the unfavorable change in ED utilization in the early adopting region was measured in comparison
with the rate of decreased utilization in other regions, which had higher historical rates of utilization.
Interviewed Providers
In each state, senior Medicaid and behavioral health officials identified and assisted in recruiting
interviewees from among provider organizations who collectively have sought to advance clinical
integration across various settings and an array of subpopulations. The profiled organizations, as a
BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 5
result, include many leading-edge providers with valuable insights on the lessons, challenges, and
benefits of clinical integration, though this group is not representative of the full range of provider
experiences related to transitioning to integrated financing models.
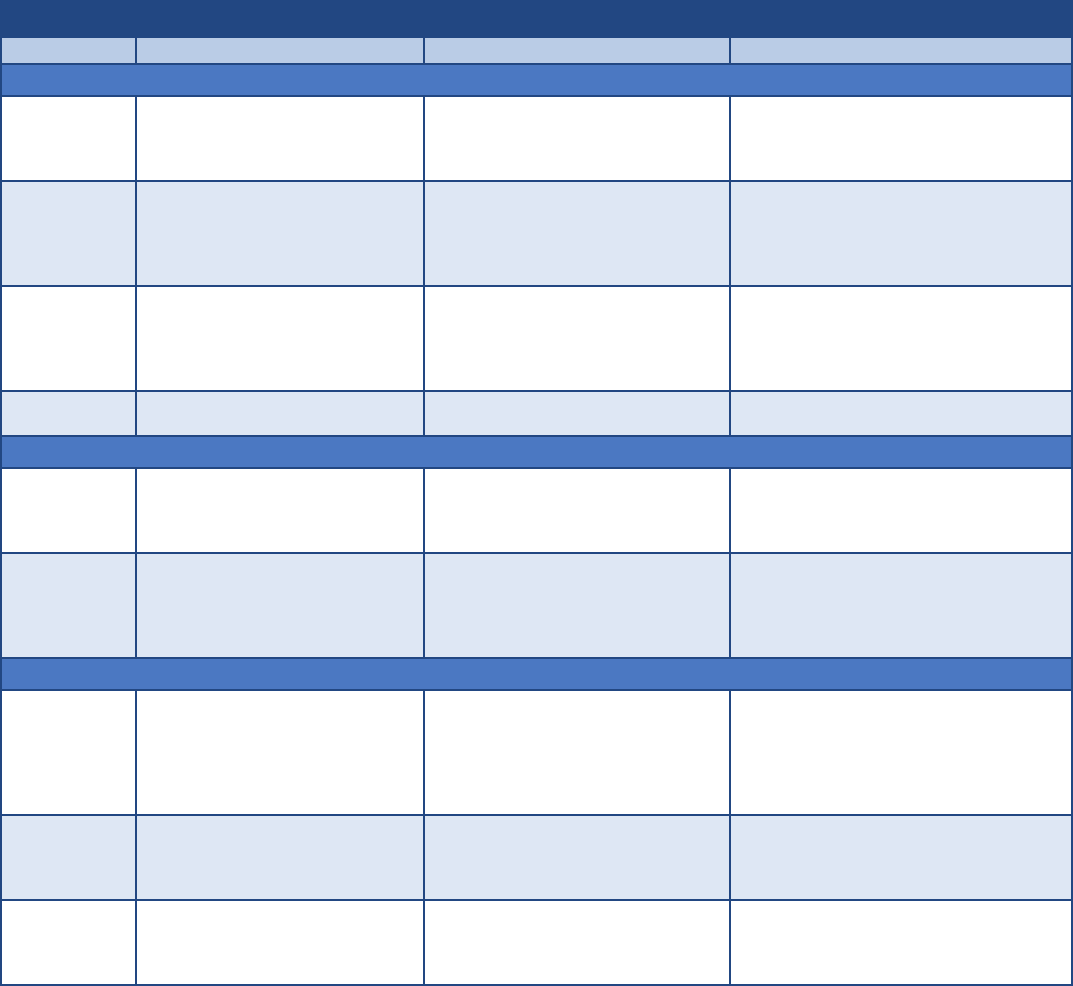
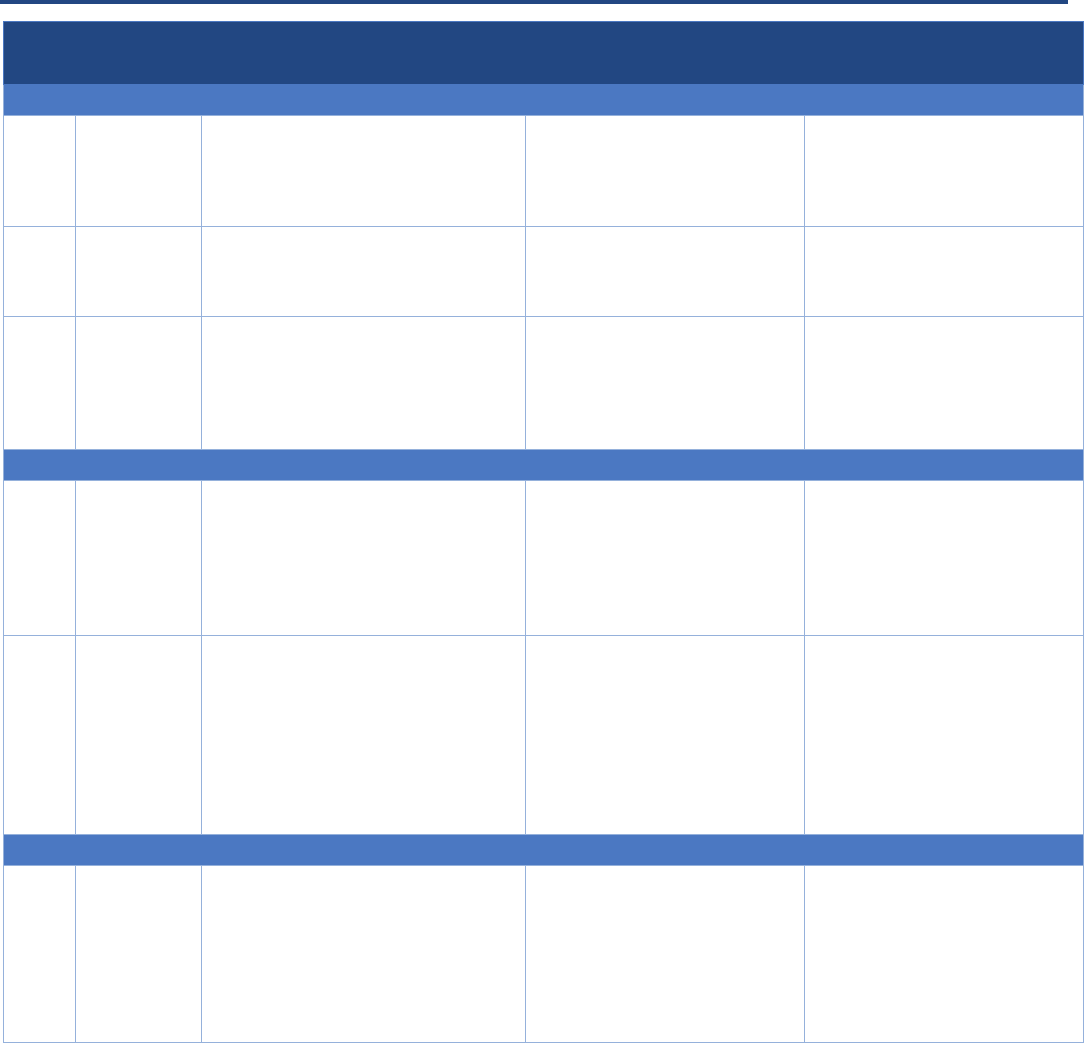
As summarized in Table 1, the interviewed providers had different lengths of experience working
with integrated managed care plans ranging from six weeks to six years, and included providers
serving adults and children and delivering an array of primary care, mental health, and SUD services.
Table 1. Interviewed Providers
Provider
Population Served
Services Provided
Transition(s) to Integrated Managed Care
ARIZONA
Children’s
Clinics
More than 5,000 children with
complex chronic diagnoses, primarily
children with Children’s Rehabilitative
Services (CRS) conditions
16
Primary and mental health care for
families, rehabilitative therapies,
pediatric specialty care, and
multidisciplinary clinics
2013. CRS members began receiving services
managed by one statewide integrated CRS
plan; as of 2018, services for CRS members
are managed by integrated ACC plans
Partners in
Recovery
More than 8,000 adults with SMI
Mental health services including
assertive community treatment (ACT),
psychosocial rehabilitation/peer
services, primary care, and health and
wellness services
2014. Members with SMI began receiving
services managed by integrated RBHA
Bayless
Integrated
Healthcare
More than 20,000 adults and children
for primary care including children
with mild to severe behavioral health
needs and adults with mild to
moderate behavioral health needs
Behavioral health services including
substance use, primary care, and
school-based physical and behavioral
services
2018. Adults and children received services
from integrated ACC plans; previously, adults
and children received behavioral health
services through a RBHA while and physical
health services through another MCO
Happy Kids
Pediatrics
More than 40,000 children
Primary care
2018. Most children began receiving services
managed by integrated ACC plans
NEW YORK
Institute for
Community
Living (ICL)
More than 10,000 adults and
children, including individuals with
mental illness and intellectual and
developmental disabilities
Mental health, supportive services, and
service-enriched housing*
2015. New York City region transitioned to
integrated MCOs and HARPs
Access:
Supports for
Living
More than 8,000 children and
families with mental illness,
substance use disorders, and/or
intellectual or developmental
disabilities
Behavioral health services (including all
Certified Community Behavioral Health
Clinics services), care management,
supportive services, and service-
enriched housing*
2016. New York State (non-New York City)
transitioned to integrated MCOs and HARPs
WASHINGTON
Clark County
Community
Services
As a county government agency,
serve the more than 465,000
residents of Clark County
Funder of non-Medicaid mental health
and SUD services, housing and
homeless services, permanent
supportive housing, and other services;
directly manage crisis responder
services
April 2016. Region transitioned to fully
integrated managed care
Catholic
Charities of
Central
Washington
More than 3,000 children and adults
Counseling and behavioral health
services, family support services, early
learning and child services, and
affordable housing*
January 2018. The North Central region
transitioned to fully integrated managed care
Mid-Valley
Clinic
Children and adults
Multispecialty clinic certified as rural
health clinic delivering primary,
specialty, and surgical care as well as
behavioral health services
January 2019. County transitioned to fully
integrated managed care
* Also partners with a federally qualified health center to deliver integrated physical and behavioral health care in at least one
clinical setting.

BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 6
Provider Insights on the Impact of Integrated Managed Care
on Clinical Integration
All nine interviewed providers have embraced new opportunities to better integrate care in their
clinical settings to more effectively serve patients with physical and behavioral health needs. Many
interviewees said their state’s transition to integrated financing facilitated provider-level data-
sharing, quality measures, and aligned financial incentives. Those improvements accelerated clinical
integration and care coordination; however, the extent of this acceleration depended on a wide
range of factors, including the state’s approach to integration, the underlying managed care and
policy environments, and characteristics of the local delivery system.
Following is a discussion of three levers that are critical for driving clinical integration in new
financially integrated programs: (1) integrated data-sharing and quality measures; (2) payment and
business practices, and (3) integrated clinical service delivery. Each section includes examples of
strategies that promote integration; as well as challenges that need to be addressed to fully embrace
these changes in new integrated models. Finally, each section concludes with several policy
recommendations for states to consider as they design and implement integrated programs.
1. Integrated Data-Sharing and Quality Measures
Financial integration creates a lever for plans and providers to share more comprehensive data
about patients’ physical and behavioral health diagnoses, utilization, referrals, and treatment plans,
because health plans now have access to data across a broader continuum of services. Providers can
use integrated data to better understand the array of patient needs; assess the gaps in care
;
coordinate treatment plans; identify high-cost, high-need patients; and develop targeted quality
improvement activities. Plans can use comprehensive data from providers to support providers’
activities to better coordinate and close gaps in care as well as to develop and refine performance
measures and financial incentives. However, while all providers interviewed spoke about the
importance of bidirectional exchange of data to better manage consumer needs, the extent to which
providers’ access to data increased after a transition to integrated managed care varied. Factors that
improved providers’ access to and use of data include: (1) partnerships and infrastructure that
enable information-sharing with managed care plans; (2) investments in health information
exchanges; and (3) plan-provider collaboration on developing integrated quality measures to enable
greater accountability for performance.
Data-Sharing with Integrated Managed Care Plans
Some behavioral health providers said that the transition to integrated financing had a rapid and
game-changing impact on data-sharing, noting that they began receiving data from plans and thus
could more effectively identify and engage high-need patients. In Arizona, leadership at Partners in
Recovery said that in the previous system of carved-out behavioral health services, providers had
limited access to physical health data, and thus, “we were blind to half of the conditions that our
patients have.” Following the transition to integrated RBHA plans for adults with SMI, Partners in
Recovery immediately began receiving primary and acute care utilization data. These data
uncovered, for example, that one Partners in Recovery patient had visited the ED 96 times in the
past year, with 24 inpatient admissions — and that Partners in Recovery providers had never known
BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 7
about these visits. Now, Partners in Recovery can identify and engage patients at high risk for acute
care utilization to find alternatives to visiting the ED. Similarly, Catholic Charities in Washington
began receiving extensive encounter data following the transition to fully integrated managed care,
including from local jails that shared data with integrated MCOs. Catholic Charities can now
proactively engage patients with behavioral health conditions such as SUDs immediately after law
enforcement encounters.
The experience of real-time data-sharing was not universal, however. Some providers in states that
had transitioned to integrated care within the last six months observed that newly integrated plans
may require additional time to understand behavioral health services before they can more
effectively organize and analyze data for bidirectional data-sharing with providers. There may be
system incompatibilities too. Behavioral health providers are generally less likely than physical health
providers to have or use health information technology. Among those who do use this technology,
managed care plan data systems may not be compatible with behavioral health providers’ electronic
health records (EHRs). Additionally, physical and behavioral health providers may need to redesign
their EHR not only to incorporate new data inputs across multiple provider types, but also to
highlight the specific elements most relevant for different provider types and protect sensitive data
in accordance with federal and state confidentiality regulations. Providers agreed that investments
from plans and providers will be critical to future improve data-sharing capabilities.
Most interviewed behavioral health providers experienced an increase in the number of entities that
pay for services as a result of the transition to integrated managed care, which has consequences for
data-sharing. Working with a single or small number of integrated plans, as opposed to a large
number, may offer opportunities to improve data-sharing through closer plan-provider
collaboration. In Arizona, Partners in Recovery works primarily with one integrated RBHA. These two
organizations partnered to develop a population health platform using comprehensive clinical and
claims data, allowing Partners in Recovery to “accelerate the use of data for care management in
ways that were unimaginable before an integrated RBHA.” On the other end of the continuum, a
provider working with more than 10 different MCOs in another state described significant challenges
in receiving and working with data across all entities, especially when consumers frequently change
plans. As a result, this provider is reliant on older claims data, limiting effectiveness to inform
interventions.
Leveraging Health Information Exchanges
Providers reported multiple benefits of participating in information-sharing through a state
electronic health information exchange (HIE), and highlighted the importance of real-time hospital
data alerts to better identify and engage high-risk patients. In 2016, all three of Arizona’s integrated
RBHAs invested in a statewide plan to integrate physical and behavioral health data in the HIE, which
also exempts behavioral health providers from participation fees.
17
The state has reported significant
increases in behavioral health provider participation in this HIE.
18
In Arizona, when Partners in
Recovery providers receive an HIE alert that a patient has visited a hospital, they immediately
communicate with that hospital to understand the underlying reasons for the visit and intervene, if
necessary, to help the patient access care in the most appropriate setting. In New York, the
statewide HIE connects regional health information organizations to store and share electronic
health data.
19
Access: Supports for Living (Access) in New York is an early adopter of the regional HIE

BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 8
and can pull real-time utilization data to target patient outreach. Each morning, Access receives an
email listing of all patients who presented at a hospital the previous evening, and clinical leaders
then participate in a morning huddle to discuss these patients and develop strategies for follow-up
care to prevent readmissions. Additionally, the HIE allows Access to see data on recent inpatient
discharges and the New York State Office of Mental Health database provides data on quality
measures, so staff can focus on engaging patients at risk for gaps in care. For example, staff now use
these systems to proactively engage individuals who are prescribed anti-psychotics and have not
received clinical testing for diabetes.
Quality Measures
Increased data-sharing can improve accountability
for provider performance. Providers, often in
collaboration with integrated plans, are using new
approaches to evaluate consumer outcomes across
physical and behavioral health domains and across
different service lines. For leaders at Access in New
York, using Healthcare Effectiveness Data and
Information Set (HEDIS) quality measures to
understand the impact of the behavioral health
services they provide on physical health outcomes
served as a “real awakening for us to think about
whole health care, and changed how we measured
our outcomes.” Leadership at Bayless Integrated
Healthcare in Arizona described using HEDIS
measures to assess the effectiveness of different
evidence-based mental health treatment practices
for patients with co-occurring conditions.
Increased access to data can also support the
design of clinical processes that may improve
consumer health and quality of life outcomes. While managed care plans have a long history of using
a robust set of physical health data to assess the quality of physical health services and measure
outcomes, they may have a steep learning curve in understanding how behavioral health services —
and integrated care — can affect both physical and behavioral health outcomes. In newly integrated
systems, providers can leverage robust data on physical and behavioral health to build more
effective partnerships with plans and capture the interconnectedness of physical and behavioral
health in care models.
Using Quality Measures to Drive Integrated Care
For Catholic Charities
in Washington State,
the transition to fully
integrated managed
care led to a focus on
developing a new
“whole person care data set” designed to track outcomes
related to integrated health care. This data set includes
relevant measures related to physical and behavioral health
conditions as well as social determinants of health (SDOH)
and patient activation measures (PAM) to assess self-care
and advocacy. Catholic Charities plans to work with its
integrated MCOs to incorporate HEDIS measures into this
data set, and use its performance on these quality measures
in negotiating risk contracts.
BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 9
Data and Quality Measures: Policy Recommendations for States
Access to integrated physical and behavioral health data is critical for providers to effectively meet the needs of
patients with co-occurring conditions. Interviewees offered many insights on how to most effectively leverage newly
available data from integrated managed care plans as well as from other providers to improve the clinical delivery of
care. Additionally, many noted that their abilities as providers to access and analyze integrated data, and to be
assessed on specific quality measures, will help integrated plans more effectively understand the impact of
behavioral health services on health outcomes and improve value-based payment reforms for behavioral health
providers. Following are data and quality measure recommendations for states to consider in designing and
implementing integrated managed care:
1. Facilitate the development of robust data-sharing protocols between integrated plans and providers prior to the
launch of integrated plans.
2. Invest in behavioral health provider readiness on data-sharing and interoperability, including design and
adoption of electronic health record systems for integrated care.
3. Invest in electronic health information exchange across medical, behavioral health, and acute care providers to
enable all providers to most effectively coordinate and reduce gaps in care.
4. Consider the impact of the number of integrated plans on provider data-sharing and ability to be held
accountable for patient outcomes.
5. Develop a quality measure set, with stakeholder input, including process and outcomes measures that
collectively assess accountability for meaningful outcomes for individuals with physical and behavioral health
needs. These measures should be included in integrated managed care plan contracts as appropriate.
2. Payment and Business Practices
With the appropriate financial, infrastructure (such as billing, data collection and reporting, and
information technology), and human resource supports in place to adopt new payment and business
models, payment levers can accelerate providers’ capacity to deliver integrated care. While not all
state transitions to integrated financing models included changes to provider payment structures at
the outset, integrated financing can better align system incentives to deliver integrated care and
promote provider accountability for managing a more complete range of services. Interviewees
noted that following transitions to integrated care, many pursued different business practices, such
as participating in state incentive programs, implementing value-based payment (VBP)
arrangements, and developing new business relationships. Finally, many providers identified
opportunities for states to mitigate administrative burden related to the transition to integrated
managed care, which may be particularly relevant for behavioral health providers that have not
previously worked with managed care.
Incentive Programs and Value-Based Payment Arrangements
Interviewees described the transformative potential of new payment models, including state
incentive programs and value-based contracts, to support their efforts to improve health outcomes
through clinical integration. AHCCCS launched the Targeted Investments Program through a 2017
amendment to Arizona’s section 1115 demonstration beginning in 2016, and invested $300 million
BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 10
to support both physical and behavioral health providers in developing the infrastructure for
integrated care.
20
Participating providers receive incentive payments annually, contingent on
meeting milestones applicable to their provider type. (See Appendix 2 for additional information
about Targeted Investments provider eligibility requirements, milestones, and payments.)
Interviewees said this program effectively incentivizes communication protocols between medical
and behavioral health providers and care coordination for high-risk patients. Physical and behavioral
health providers work toward different milestones, but also have opportunities to work together to
improve care and receive incentive payments. Providers highlighted the importance of collaborating
to define high-risk patients and identify areas of clinical overlap where both types of providers could
improve care.
In other states, even where state policy has largely maintained existing payment structures,
partnerships with integrated managed care plans are allowing some behavioral health providers to
begin participating in VBP arrangements that incentivize clinical integration. For example, although
the transition to integrated care continued the underlying fee-for-service payment system for
behavioral health provider payments, New York concurrently rolled out an extensive VBP initiative
that included a number of voluntary opportunities to promote incentives and accountability for
integrated care.
21
Access participates in Coordinated Behavioral Health Services, a behavioral health
independent practice association (IPA) focused on integrated behavioral and physical health. It also
holds a value-based contract with an integrated MCO that will shift later this year to an arrangement
with both upside and downside risk. Also in New York, Institute for Community Living has partnered
with Healthfirst (an MCO that offers a HARP plan) in a HARP VBP pilot.
22
Representatives of both
providers said that they have improved health outcomes and are better-prepared to participate in
future VBP arrangements because of their participation in these arrangements.
Other providers have worked closely with their integrated managed care plans, and in some cases
with their state Medicaid agency, to develop and refine VBP arrangements that advance integrated
physical and behavioral health services. Plans may also be able to make investments in critical
capacity areas that allow providers to meet requirements for new payment models, such as
information technology, and data collection and reporting capacity. Bayless Integrated Healthcare in
Arizona has value-based contracts with most ACC plans, and has worked closely with these plans to
educate them about behavioral health care models, payment rates, and coding practices, among
other things, to develop financially sustainable contract terms. Similarly, Children’s Clinics in Arizona
has collaborated with plans and AHCCCS to develop behavioral health quality measures for VBP
models. As part of this effort, Children’s Clinics negotiated a wraparound rate for key behavioral
health services that were not previously reimbursable. Similarly, Partners in Recovery in Arizona
receives incentive payments from its partner RBHA based on physical health performance measures
such as increasing the number of patients with diabetes who receive an annual retinal eye exam. To
achieve this objective, Partners in Recovery now works with a local optometrist and coordinates
appointments for their clients within their clinics.
BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 11
New Business Relationships
Adoption of new integrated financing models can drive physical and behavioral health providers to
explore new partnerships. In 2018, Arizona’s Happy Kids Pediatrics began working with integrated
ACC plans in 2018, and also established a partnership with a behavioral health provider to offer co-
located physical and behavioral health services to more effectively meet the behavioral health needs
of its patient population. The potential for incentive payments from the Targeted Investments
Program strengthened the business case for this new collaboration. For pediatric primary care
providers such as Happy Kids Pediatrics, the Targeted Investments Program outlines 20 core
components and related milestones tied to provider payments to advance the objective of
integrating primary care and behavioral health services for both preventive and chronic illness
care.
23
For example, milestones require communications and care management protocols with other
providers and with MCOs, and patient attestations that warm hand-offs for newly identified
behavioral health needs occurred 85 percent of the time. Other milestones require the development
of practice-specific action plans to improve integration, using the Standard Framework for Levels of
Integrated Healthcare continuum
24
to track progression between coordinated, co-located, and
integrated levels of care. These milestones, among others, incentivize practices such as Happy Kids
Pediatrics to enter into these partnerships.
Additionally, multiple providers interviewed across different states have partnered with federally
qualified health centers (FQHCs) to create integrated practices. The Institute for Community Living in
New York recently partnered with an FQHC to develop an integrated health hub, which includes
primary care, mental health, care management, and a family resource center. Still however, in these
partnerships, the physical and behavioral health providers may be using different EHRs, and
providers are exploring different approaches to addressing this challenge.
Provider Payment and Business Practice Challenges
The experience of behavioral health providers transitioning to integrated managed care is shaped by
the previous mechanisms under which they reimbursed for mental health and/or SUD services. (See
Appendix 2 for additional detail on how behavioral health provider payment mechanisms changed
related to the transitions for specific populations by state.) In states where providers previously
received payment from a single entity for services or via a block grant, transitioning to working with
private plans as well as multiple payers can lead to administrative challenges. For example, some
behavioral health providers transitioning to integrated managed care experienced revenue issues in
the months immediately following the transition. They also described increased rates of claims
denials and delayed payments until they became familiar with all of the specific processes and
requirements of different integrated MCOs. While many of these issues were resolved in the months
immediately following the transition, some providers reported ongoing administrative burden to
manage billing with multiple plans, and identified the need to hire additional administrative support
staff to process encounters in accordance with the requirements of each integrated plan.
Some providers, especially smaller behavioral health providers, may have limited financial resources,
which may impede their ability to meet the data, reporting, and billing requirements of working with
managed care plans. Mergers may help providers manage these financial challenges by improving
access to supporting infrastructure, creating economies of scale, and increasing negotiating power.
BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 12
Some interviewees described the financial pressures on smaller behavioral health providers in a
changing market with evolving payer and provider relationships, and noted that integrated financing
may have the effect of accelerating consolidation of the behavioral health provider market.
Even as Medicaid agencies move toward integrated financing, other state policies and procedures
can impede capacity to develop new service lines and business models. Some providers described
challenges becoming credentialed with plans to provide both physical and behavioral health services,
even though they had integrated licenses. One behavioral health provider struggled to secure
primary care credentials from the integrated MCOs, which contributed to the decision to partner
with an FQHC to set up an integrated clinic.
Payment and Business Practice Reforms: Policy Recommendations for States
Many providers have pursued new payment and business arrangements that facilitate clinical integration. However,
some behavioral health providers described “living in the gap” between focusing on improved outcomes and quality
measures and being paid for fee-for-service encounters. Providers identified greater opportunities for integrated
managed care plans to pay for value. Following are payment and business practice reform recommendations for
states to consider in designing and implementing integrated managed care:
1. Develop methodologies inclusive of behavioral health services in VBP models that incentivize high-value
integrated care.
2. Invest in provider readiness and system capacity to participate in VBP arrangements, tailoring this support to
the unique considerations of smaller behavioral health providers.
3. Develop state-administered incentive or other investment programs to foster clinical practice changes, build
system infrastructure and capacity to enable integrated care delivery, and improve communication between
physical and behavioral health providers.
4. Consider the impact of the number of integrated plans on provider contracting and administrative burden.
5. Identify needed reforms to licensing and credentialing to enable providers to deliver and be paid for integrated
care.
3. Integration in Clinical Service Delivery
Across care settings and patient populations, integrated financing has created new opportunities and
energy for interviewed providers to move toward clinical integration of physical and behavioral
health services to more effectively meet the needs of their patients. The focus of clinical changes
varied among providers interviewed, and included service and staffing redesign, screening and
assessment practices, care coordination, and interventions to address SDOH. Providers are
leveraging new data-sharing opportunities, payment incentives, and partnerships with managed care
plans and other providers to accelerate their ability to deliver integrated care that encompasses
physical and behavioral health as well as social needs. States can create policies to further drive
these activities, including streamlining oversight activities at the state level, making investments or
using plan requirements that encourage investments in provider training and capacity building, or
developing incentives to drive integration at the service delivery level.
BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 13
Service and Staffing Redesign
After transitioning to working with integrated plans, many providers have increased their capacity to
deliver integrated care by redesigning the services delivered and staffing arrangements. When
Partners in Recovery in Arizona began working with an integrated RBHA, it introduced primary care
into its behavioral health settings, and focused on increasing member engagement around physical
health and wellness. Partners in Recovery used newly available data on its patient population from
the RBHA to identify opportunities to impact modifiable health behaviors, and subsequently
established a teaching kitchen and fitness center where newly hired staff lead cooking and exercise
classes. As a result of the transition to fully integrated managed care, Catholic Charities in
Washington State redesigned services around the holistic needs of the communities it serves to
improve the quality of care, including using patient surveys to inform quality improvement and hiring
a client services manager. This initiative has increased its ability to deliver earlier interventions for
populations with rising risk.
Some providers have focused on expanding
integrated care delivery to new settings. Several
providers have pursued partnerships to allow
them to open clinics with co-located physical and
behavioral health services. For example, since
opening the East New York Health Hub in
partnership with the Community Healthcare
Network, an FQHC, Institute for Community Living
reported that many of its patients who were
previously disconnected from primary care
providers can now have same-day visits, resulting
in improved access to preventive care. Also in New
York, Access partners with an FQHC on an
integrated clinic for individuals with serious
behavioral health needs, and has recently
expanded its offerings to include SUD services,
including medication-assisted treatment. Access is
in the process of opening two behavioral health
urgent care centers to help individuals with acute
needs access high-quality care outside of an ED
and then engage in ongoing treatment. In Arizona,
the transition of children’s behavioral health to integrated ACC plans led Bayless Integrated
Healthcare to partner with plans on developing integrated school-based clinics. Services delivered at
these clinics include primary care, psychiatry, therapy, and wellness coaching with a focus on
destigmatizing children and families with mental health needs. Developing these clinics to provide
comprehensive care for the whole family only became financially viable when they could reimburse
to the same MCO for an entire family’s physical and behavioral health services. Before, the siloed
funding streams for children and adults limited its ability to serve children.
Bridging Differences Across Providers
Providers need to bridge
cultural as well as clinical
differences to integrate
physical and behavioral
health models of care.
At Children’s Clinics in Arizona, leadership observed that
behavioral health providers often contributed expertise in
holistic assessments of individual and family situations, while
physical health providers were more experienced with
tracking data and outcomes. Creating integrated teams
requires leadership to merge these different strengths and
perspectives and foster open and productive communication
and education. These integrated provider teams —
particularly care coordination staff — benefit from training
on these varying approaches to care and the continuum of
physical and behavioral health needs.
BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 14
Screening and Referrals
While most physical and behavioral health providers have historically only screened their patients for
the needs that they themselves treat, many providers reported that they now use more expansive
screenings that are required by the state as part of their contracts with MCOs. For example, Catholic
Charities in Washington State includes questions about physical and behavioral health as well as
family situations and SDOH. In Arizona, Children’s Clinics leadership said that they introduce these
conversations to patients by saying, “We’re going to ask you questions that you’ve never been asked
before, and you will see providers you never thought you would see all at the same time. Your
appointment has to be a little longer now, but we’re doing this because we think it’s going to give
you a better life.” One provider, however, cautioned that lengthy intake appointments could deter
consumers from accessing care. Interviewees said that intakes may require two hours to complete,
and that they are looking for opportunities to increase efficiency while also capturing vital
information.
Beyond initial assessments, many providers are incentivized under integrated managed care to
conduct periodic screenings. In particular, behavioral health providers have an increased focus on
screening patients for chronic physical health conditions. When an assessment identifies an unmet
need, providers strive for warm handoffs to the appropriate staff or external providers with referrals
and patient follow-ups as needed. Arizona has developed guidance and specific targets for
assessments and management of identified high-risk populations for participating providers in the
Targeted Investments Program. One participating provider, Happy Kids Pediatrics, used to refer
patients with behavioral health needs to external providers, but would not receive any follow-up
information afterward. Now, in response to Targeted Investments measures, they conduct a warm
hand-off to their co-located behavioral health partner and ensure that a patient is seen within five
days to receive the full intake and develop a treatment plan.
Integrated Care Plans and Care Coordination
When held accountable for quality measures and closing gaps in care across all health needs, some
providers have invested in integrated care planning and coordination within their clinical practices.
Many of the interviewed providers produce a single integrated care plan across all health needs and
conduct weekly care coordination meetings with both physical and behavioral health staff to discuss
the highest-risk patients. Integrated service plans, created by physical and behavioral health
providers as well as patients and family members, have “transformed the quality of care that a
family receives,” said a Children’s Clinics interviewee. These plans equip all providers with the
necessary understanding of patient goals and treatment plans across different clinical practices. At
Partners in Recovery, clinicians collaborate on patient-centered integrated care plans for high-need
patients. These plans draw on the organization’s innovative approach of using functional behavioral
assessments to review high-utilizers’ ED records, and incorporate input from patients, family
members, and other providers to better understand the root causes for preventable ED visits.
Providers pursuing integrated care also more actively engage other treating providers or other
partners to ensure that patients experience well-coordinated care. Partners in Recovery promotes
coordination between physical and behavioral health providers through daily integrated care
touchpoints to discuss all patients coming in that day. Access in New York now provides care

BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 15
management services in EDs and focuses on care transitions when patients leave acute care settings,
including by coordinating care with peer service organizations when a patient leaves a psychiatric
hospitalization. As discussed in the earlier section on integrated data-sharing and quality measures,
Access conducts daily huddles to discuss patients admitted the previous night, as well as weekly
huddles with partner organizations to coordinate care for individuals with complex needs or with a
gap in their physical health quality indicators, such as a missing screening. New partners include child
welfare services staff who join huddles for high-risk children. Finally, when working across multiple
provider types and equipped with comprehensive data, providers can conduct real-time medication
reconciliation for prescribed medical and psychotropic medications.
Additionally, many states pursuing integrated
managed care require newly integrated MCOs to
conduct more robust coordination of care
management at the plan level, especially for high-
need populations. Liaisons from MCOs worked on-
site at the Arizona-based Children’s Clinics to meet
with patients and coordinate care, and other
interviewed providers described closely
collaborating with MCO care management staff.
Providers cited the value of MCO care
management in identifying gaps in care,
coordinating patient outreach, and addressing
patient questions related to plan coverage or
communications.
Social Determinants of Health
For many providers, transitioning to integrated
physical and behavioral health has also led to
greater organizational focus on SDOH. In addition
to incorporating questions related to SDOH on
screenings and assessments, providers frequently
identified new service delivery initiatives to
address SDOH. While some providers, such as the
Institute for Community Living in New York, have
long offered supportive housing services, others
are expanding their work in this area. In
Washington State, the Medicaid agency created
Accountable Communities of Health (ACH) within each region to better align health resources to
improve health and address all medical, behavioral, and social needs. ACHs engage a broad group of
stakeholders from different sectors and communities and offer training to providers.
25
Providers
there said ACHs centralize resources to address SDOH in clinical work, as well as in aggregate data
and inform regional planning on issues related to SDOH. The Mid-Valley Clinic, a North Central
Washington rural health clinic in early stages of integrating behavioral health services, described
Expanding the Focus on Social
Determinants of Health
Leadership at Clark County Community
Services (Clark County) in Washington
State bring a unique perspective on
how the transition to integrated
managed care can affect the resources
allocated to address social
determinants of health. As the social
service agency in county government,
Clark County previously managed multiple funding sources
for behavioral health services. When many of these funding
sources were moved to integrated MCOs or the regional
Behavioral Health Administrative Service Organization, the
county experienced greater flexibility to target their local
behavioral health funding to initiatives that address social
determinants of health. This new organizational flexibility
mirrored a broader commitment, across plans and providers,
to ensure that the care delivered extends beyond the clinic
walls. County leadership noted that “care integration is
bigger than just physical health and behavioral health; it is
about whole person care,” as one of the most significant
impacts of the transition to fully integrated managed care.
BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 16
these ACH trainings as very valuable. The trainings and resources also equip organizations with
practical skills such as motivational interviewing for integrated care coordination.
Integrated Clinical Service Delivery: Policy Recommendations for States
Interviewees say delivering integrated care has led to service delivery transformations to address physical and
behavioral health needs as well as SDOH. Many providers noted opportunities for states to more effectively support
these efforts in the transition and implementation of integrated managed care. They also underscored the
foundational importance of data-sharing and payment reforms to help them transform clinical care delivery.
Following are recommendations related to clinical service delivery for states to consider in designing and
implementing integrated managed care:
1. Invest in provider training and capacity-building for clinical integration to foster adoption of evidence-based and
promising practices. Consider assigning responsibility for clinical integration to a single statewide agency to
ensure that providers can access available resources.
2. Collaborate with providers and managed care plans to develop guidance on integrated screenings and other
assessments that align with quality measures. Develop infrastructure for providers to share assessment
information to avoid duplication of efforts.
3. Ensure that consumers with co-occurring physical health, mental health, and SUD needs can receive same-day
services and coordination for multiple conditions. States might consider requirements that managed care plans
facilitate integrated care management.
4. Incentivize the development of integrated service plans across physical and behavioral health needs, with
requirements to engage patients and families.
5. Provide comprehensive monitoring and oversight of access to integrated care as well as all quality measures to
identify any disparities in the care delivered.
6. Identify opportunities for providers to incorporate assessments and interventions related to SDOH into their
service delivery, and, where applicable, consider the unique role for county-based entities in coordinating
planning and service delivery related to SDOH and social needs.
Looking Ahead
States interested in developing or refining integrated managed care models can glean valuable
lessons both from the emerging evidence in formal evaluations of patient outcomes in integrated
systems, and from the on-the-ground experiences of providers in these systems. Providers have
identified important elements in the design and implementation of effective integrated programs,
from data-sharing to payment mechanisms to specific interventions to foster integrated clinical
delivery. These broad considerations reflect the importance of thoughtful design of physical-
behavioral health integration initiatives, including managed care plan requirements and state
policies that will shape providers’ ability to integrate care at the clinical level.
BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 17
ACKNOWLEDGEMENTS
The authors would like to thank the leaders at provider organizations who contributed their time and expertise to
inform this brief: Amy Anderson-Winchell, President and Katariina Hoaas, Chief Clinical Officer, Access: Supports for
Living; Justin Bayless, Chief Executive Officer, Bayless Integrated Healthcare; Marco Carrasco, Jr., Chief Integration
Officer, Happy Kids Pediatrics; Becky Corson, Clinic Administrator, Mid-Valley Clinic; Chris De Villeneuve, Division
Director of Mental Health Services, Catholic Charities of Central Washington; Christy Dye, Chief Executive Officer,
Partners in Recovery; Vanessa Gaston, Director of Clark County Community Services; Jared Perkins, Chief Executive
Officer, Children’s Clinics; David Woodlock, Chief Executive Officer, Institute for Community Living. The authors
would also like to thank George Jacobson and Dana Hearn of the Arizona Health Care Cost Containment System,
Alice Lind at the Washington Health Care Authority, and Robert Myers at the New York State Office of Mental Health
for contributing to the development of this brief.
ABOUT THE CENTER FOR HEALTH CARE STRATEGIES
The Center for Health Care Strategies (CHCS) is a nonprofit health policy resource center committed to improving
health care quality for low-income Americans. CHCS works with state and federal agencies, health plans, providers,
and community-based organizations to develop innovative programs that better serve people with complex and high-
cost health care needs. For more information, visit www.chcs.org.
BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 18
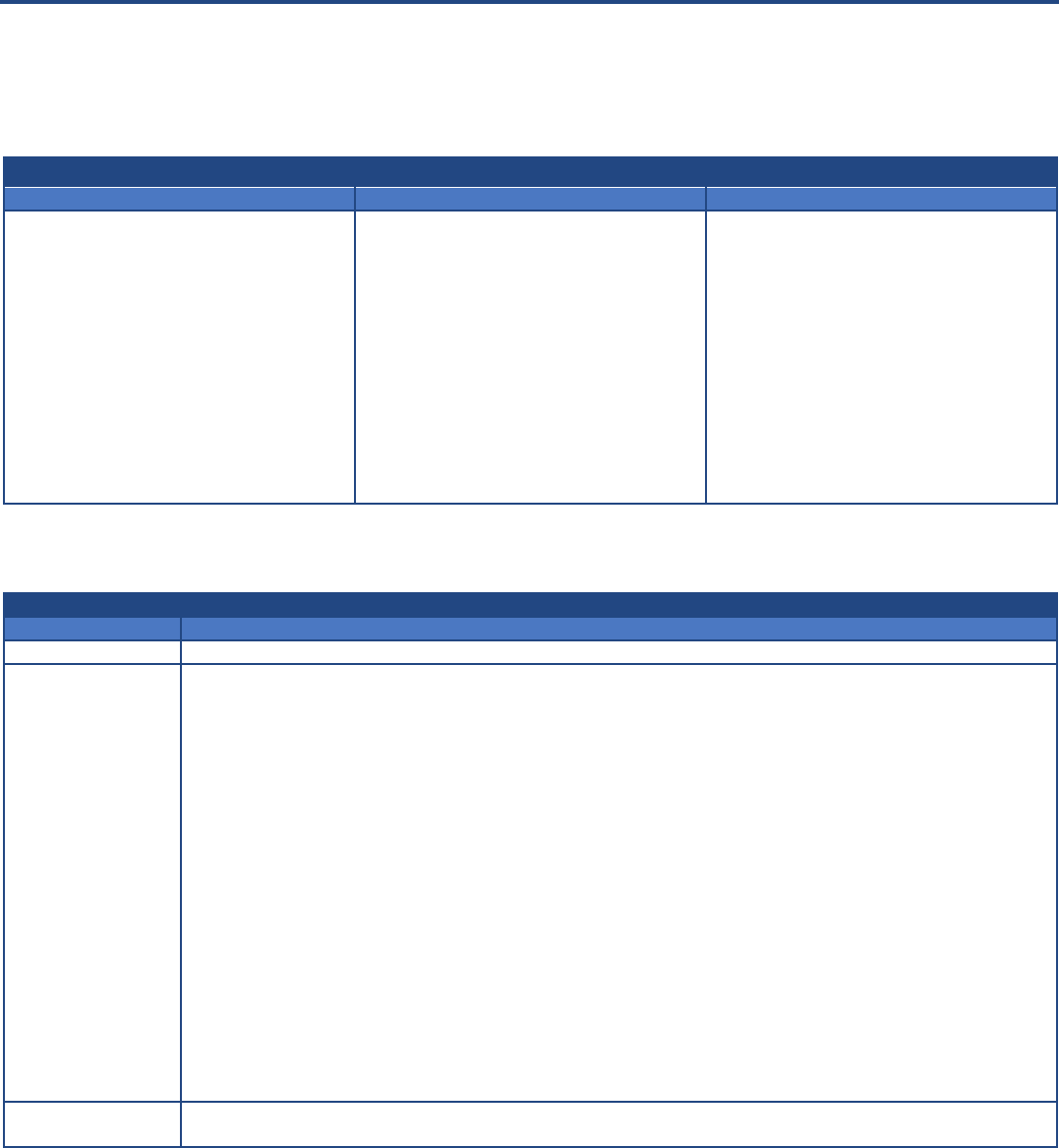
Appendix 1. Summary of Transition to Integrated Managed Care in Profiled States
Year
Population
Overview of State Approach
Primary behavioral health
provider payment mechanisms
before transition
Primary behavioral health
provider payment mechanisms
after transition
ARIZONA*
2013
Children’s
Rehabilitative
Services (CRS)
Enrollees
Integrated all physical, behavioral, and
CRS specialty services to be managed by
a single statewide MCO.
Providers received payments from
a statewide CRS plan for specialty
CRS services, and single regional
RBHAs for behavioral health
services.
Providers receive payments from
a single statewide MCO for
primary, specialty, and behavioral
health services.
2014 -
2015
Enrollees
with SMI
Integrated all physical and behavioral
health services to be managed by an
integrated RBHA, with one integrated
RBHA available in each region.
Providers received payments from
single regional RBHAs for specialty
behavioral health services.
Providers receive payments from
single regional integrated RBHAs
for primary and all behavioral
health services.
2018
General Adult
(non-SMI)
and Children
**
Integrated all physical and behavioral
health services to be managed by an
integrated ACC plan, including adults
with mild to moderate mental health or
substance use needs.
Providers received payments from
single regional RBHAs for
behavioral health services for
adults with general mental health
and substance use needs and
children.
Providers receive payments from
between two and seven
integrated ACC plans for all
primary and behavioral health
services for this population.
NEW YORK
2015 -
2016
Adults
Integrated all physical and behavioral
health services for adults to be managed
by an integrated MCO, which could be
either a mainstream Medicaid managed
care plan or a HARP.*** The number of
available plans varies by region, with up
to 11 plans in the New York City region.
Providers received payments from
mainstream MCOs for mild to
moderate behavioral health
services, and from the state
Medicaid agency for specialty
behavioral health services.
Providers receive payments from
integrated MCOs (mainstream
MCOs or HARPs) for all physical
and behavioral health services.
2019
Children
Began transition of children into
integrated mainstream MCOs and
HARPs in 2019, which requires
transitioning six 1915(c) waivers to an
integrated Section 1915(c) waiver and
then a Section 1115 waiver authority.
HARPs will be required to contract with
health homes for children, which began
operating in 2016.
Providers received payments from
mainstream MCOs for mild to
moderate behavioral health
services, and from the state
Medicaid agency for specialty
behavioral health services.
Providers receive payments from
integrated MCOs (mainstream
MCOs or HARPs) for all physical
and behavioral health services.
WASHINGTON
2016 -
2020
Adults
Integrated all physical and behavioral
health services for adults and children to
be managed by one of up to three
integrated MCOs, with integration
phased by region.
Providers received payments from
mainstream MCOs for mild to
moderate behavioral health
services, from the Regional
Service Network (RSN) for mental
health services, and from county
governments for SUD
Services.****
Providers receive payments from
between three and five integrated
MCOs for all physical and
behavioral health services.
* Other Arizona Medicaid enrollees either have transitioned to integrated managed care at other times (including enrollees eligible for Arizona Long-Term Care
Services, and those dually eligible for Medicare and Medicaid) or are planned to transition by 2020 (including children in foster care).
** CRS enrollees transitioned at this time from receiving coverage from a single statewide integrated CRS plan to selecting one of several available ACC plans.
*** HIV Special Needs Plans may also be integrated MCOs.
****For regions that transitioned after 2016, RSNs transitioned to become managed behavioral health organizations responsible for both mental health and SUD
services.
BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 19
Appendix 2. Arizona Targeted Investments Program
26
Arizona’s Targeted Investments (TI) Program is designed to incentivize behavioral health integration in the state’s Medicaid program.
Three types of Medicaid providers are eligible to participate: primary care, behavioral health, and hospitals, each with its own eligibility
requirements as outlined below. The TI program is authorized under AHCCCS’ Section 1115 Waiver for five years beginning in 2016.
Under the program, managed care plans provide financial incentives to eligible Medicaid providers who meet certain benchmarks for
integrating and coordinating physical and behavioral health care for Medicaid beneficiaries.
Provider Eligibility Requirements
Primary Care Provider
Behavioral Health Provider
Hospital
Providers must have a minimum assigned
AHCCCS members across all health plans
with which they are contracted.
Providers must attest to having:
An electronic health record (EHR) that
can exchange and use electronic health
information from other systems without
special effort on part of the user, and;
Completed a behavioral health
integration assessment using one of the
AHCCCS-specified tools.
Providers must have delivered an
AHCCCS-defined minimum number of
qualifying outpatient services to members
during a recent 12-month period.
Providers must attest to having:
An EHR that can exchange and use
electronic health information from
other systems without special effort on
part of the user, and;
Completed a behavioral health
integration assessment using one of the
AHCCCS-specified tools.
Hospitals must have had an AHCCCS-
defined minimum number of qualifying
member discharges across all health plans
during a recent 12-month period.
Hospitals must attest to having an EHR
that can exchange and use electronic
health information from other systems
without special effort on part of the user.
TI Payments. Financial incentives are paid on an annual basis to participating eligible providers. The table below describes how
providers can qualify to receive incentive payments for each year of the program.
TI Program Incentive Payments Timeline
Year
Payment Contingencies
Year 1 (10/16-9/17)
Contingent on acceptance into program.
Year 2 (10/17-9/18)
Year 3 (10/18-9/19)
Contingent on completing core component milestones, which vary by provider type and concentration. Below are
examples of milestones for primary care providers focused on adults with behavioral health needs.
27
For a list of
milestones for behavioral health providers and hospitals working with adult and pediatric populations, refer to the TI
years 2 and 3 core components and milestones on the TI program overview website.
28
1. Utilize a behavioral health integration toolkit and practice-specific action plan to improve integration and
identify level of integrated healthcare
2. Identify members who are high-risk and develop electronic registry; Demonstrate use of identification criteria
and document members in registry
3. Utilize care managers for members in high-risk registry; Demonstrate that care manager(s) are trained in
integrated care
4. Implement integrated care plan
5. Screen all members to assess SDOH
6. Develop communication protocols with physical health and behavioral health providers for referring members
7. Screen all members for behavioral health disorders
8. Utilize the Arizona Opioid Prescribing Guidelines for acute and chronic pain
9. Participate in the health information exchange with Health Current
10. Identify community-based resources
11. Prioritize access to appointments for all individuals listed in high-risk registry
12.
Participate in any TI program-offered training
Year 4 (10/19-9/20)
Year 5 (10/20-9/21)
Contingent on meeting or exceeding performance targets. Performance targets to be determined.
BRIEF | Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 20
1
Medicaid and CHIP Payment and Access Commission. “Integration of Behavioral and Physical Health Services in Medicaid.” March 2016. Available at:
https://www.macpac.gov/wp-content/uploads/2016/03/Integration-of-Behavioral-and-Physical-Health-Services-in-Medicaid.pdf
.
2
Medicaid and CHIP Payment and Access Commission. “Behavioral Health in the Medicaid Program—People, Use and Expenditures.” June 2015. Available
at: https://www.macpac.gov/wp-content/uploads/2015/06/Behavioral-Health-in-the-Medicaid-Program%E2%80%94People-Use-and-Expenditures.pdf
.
M.R. Burt, L.Y. Aron, T. Douglas, J.Valente, E. Lee, and B. Iwen. Homelessness: Programs and the People They Serve | Findings of the National Survey of
Homeless Assistance Providers and Clients. Urban Institute, December 1999. Available at: https://www.urban.org/research/publication/homelessness-
programs-and-people-they-serve-findings-national-survey-homeless-assistance-providers-and-clients. A. Luciano and E. Meara. “Employment Status of
People with Mental Illness: National Survey Data from 2009 and 2010.” Psychiatric Services 65, no. 10 (2014): 1201–1209. Joshua Breslau et al., “Mental
Disorders and Subsequent Educational Attainment in a US National Sample,” Journal of Psychiatric Research 42, no. 9 (July 2008): 708–716. J. Karberg and D.
James. Bureau of Justice Statistics Special Report: Substance Dependence, Abuse, and Treatment of Jail Inmates, 2002. U.S. Department of Justice Office of
Justice Programs, July 2005. Available at:
https://www.bjs.gov/content/pub/pdf/sdatji02.pdf. S.J. Prins, “Prevalence of Mental Illnesses in US State Prisons:
A Systematic Review, Psychiatric Services 65, no. 7 (July 2014): 862–872.
3
National Association of State Mental Health Program Directors. “Morbidity and Mortality in People with Serious Mental Illness.” October 2006. Available
at: https://nasmhpd.org/sites/default/files/Mortality%20and%20Morbidity%20Final%20Report%208.18.08.pdf
.
4
Medicaid and CHIP Payment and Access Commission. “Behavioral Health in the Medicaid Program—People, Use and Expenditures.” June 2015.
5
Ibid.
6
S. Melek and D. Norris. Chronic Conditions and Comorbid Psychological Disorders. Milliman, July 2008. Available at:
http://us.milliman.com/insight/research/health/pdfs/Chronic-conditions-and-comorbid-psychological-disorders/
.
7
D. Lawrence and S. Kisely. “Inequalities in healthcare provision for people with severe mental illness.” Journal of Psychopharmacology, vol. 24, 4 Suppl
(2010): 61–68.
8
C.J. Peek for The National Integration Academy Council. Lexicon for Behavioral Health and Primary Care Integration: Concepts and Definitions Developed by
Expert Consensus. Agency for Healthcare Research and Quality, 2013. Available at: http://integrationacademy.ahrq.gov/sites/default/files/Lexicon.pdf
.
9
B. Heath, P. Wise Romero, and K. Reynolds. A Review and Proposed Standard Framework for Levels of Integrated Healthcare. SAMHSA-HRSA Center for
Integrated Health Solutions, March 2013. Available at:
https://www.integration.samhsa.gov/integrated-care-
models/A_Standard_Framework_for_Levels_of_Integrated_Healthcare.pdf.
10
E. Woltmann, A. Grogan-Kaylor, B. Perron, H. Georges, A.M. Kilbourne, M.S. Bauer. “Comparative effectiveness of collaborative chronic care models for
mental health conditions across primary, specialty, and behavioral health care settings: Systematic review and meta-analysis.” American Journal of
Psychiatry, 169, no. 8 (2012): 790–804. B. Reiss-Brennan, K.D. Brunisholz, C. Dredge, P. Briot, K. Grazier, A. Wilcox, et al. “Association of Integrated Team-
Based Care with Health Care Quality, Utilization, and Cost.” Journal of the American Medical Association, 316 no. 8 (2016): 826–834.
11
State Health Access Data Assistance Center (SHADAC), University of Minnesota School of Public Health. “Catalog of Medicaid Initiatives Focusing on
Integrating Behavioral and Physical Health Care: Final Report.” July 2015. Available at:
https://www.macpac.gov/wp-content/uploads/2015/09/Catalog-of-
Behavioral-and-Physical-Health-Integration-Initiatives.pdf.
12
Bipartisan Policy Center. “Integrating Clinical and Mental Health: Challenges and Opportunities.” January 2019. Available at:
https://bipartisanpolicy.org/wp-content/uploads/2019/01/Integrating-Clinical-and-Mental-Health-Challenges-and-Opportunities.pdf
.
13
Mercer Health and Benefits, LLC. “Independent Evaluation of Arizona’s Medicaid Integration Efforts – Programs for Children’s Rehabilitative Services and
Persons Determined to Have a Serious Mental Illness.” November 2018. Available at:
https://azahcccs.gov/shared/Downloads/News/CRS_SMI_IndependentEvaluationReport_11_27_18.pdf
.
14
New York State Department of Health. “Request for Proposals #20024, Independent Evaluation of the New York State (NYS) Health and Recovery Plans
(HARP) Program and Self-Directed Care (SDC) Pilot Program.” January 2019. Available at: https://www.health.ny.gov/funding/rfp/20024/20024.pdf
.
15
D. Mancuso. Evaluation of Fully Integrated Managed Care in Southwest Washington: Preliminary First-Year Findings. Washington State Department of
Social and Health Services, August 2017. Available at: https://www.hca.wa.gov/assets/program/FIMC-preliminary-first-year-findings.pdf
.
16
The Children’s Rehabilitative Services (CRS) program was created in 1929 to serve children and youth with special health care needs. Until 2013, CRS
program services were carved out from Medicaid managed care plans. The CRS program receives grant funds under section 501(a)(1)(D) of Title V.
17
Health Current. “Regional Behavioral Health Authorities Support Statewide HIE Integration Plan.” May 2016. Available at:
https://healthcurrent.org/regional-behavioral-health-authorities-support-statewide-hie-integration-plan/
.
18
D. Bachrach, P. Boozang, H. Davis. How Arizona Medicaid Accelerated the Integration of Physical and Behavioral Health Services. Manatt Health, May
2017. Available at: https://www.manatt.com/Insights/White-Papers/2017/How-Arizona-Medicaid-Accelerated-the-Integration-o
19
New York eHealth Collaborative. “What is the SHIN-NY?” Available at: https://www.nyehealth.org/shin-ny/qualified-entities/.
20
For more information, see: Arizona Health Care Cost Containment System. Available at: https://www.azahcccs.gov/PlansProviders/TargetedInvestments/.
21
New York State Department of Health. “DSRIP – Value Based Payment Reform (VBP).” Available at:
https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/vbp_reform.htm
.
22
New York State Department of Health. “Health and Recovery Plan Value Based Payment Arrangement, Measurement Year 2018 Fact Sheet.” February
2018. Available at: https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/vbp_library/2018/docs/2018-02-09_harp.pdf
.
23
Arizona Health Care Cost Containment System. “Pediatric Primary Care Provider AHCCCS Targeted Investments Program Core Components and
Milestones, 2019.” Available at: https://www.azahcccs.gov/PlansProviders/Downloads/TI/CoreComponents/PediatricPCP_webpage.pdf
.
24
Heath, et al., op.cit.
25
Center for Community Health and Evaluation. “Regional Collaboration for Health System Transformation: An Evaluation of Washington’s Accountable
Communities of Health.” January 2019. Available at: https://www.hca.wa.gov/assets/program/cche-evaluation-report-for-ACHs.pdf
.
26
For more information, see: Arizona Health Care Cost Containment System. Available at: https://www.azahcccs.gov/PlansProviders/TargetedInvestments/.
27
Arizona Health Care Cost Containment System. “Adult Primary Care Provider AHCCCS Targeted Investments Program Core Components and Milestones,
2019.” Available at: https://www.azahcccs.gov/PlansProviders/Downloads/TI/CoreComponents/Adult_PCP_webpage.pdf
.
28
Ibid.
ENDNOTES
